What Is Biofilm? Why This Might Be the Missing Link in Your Chronic Health Issues
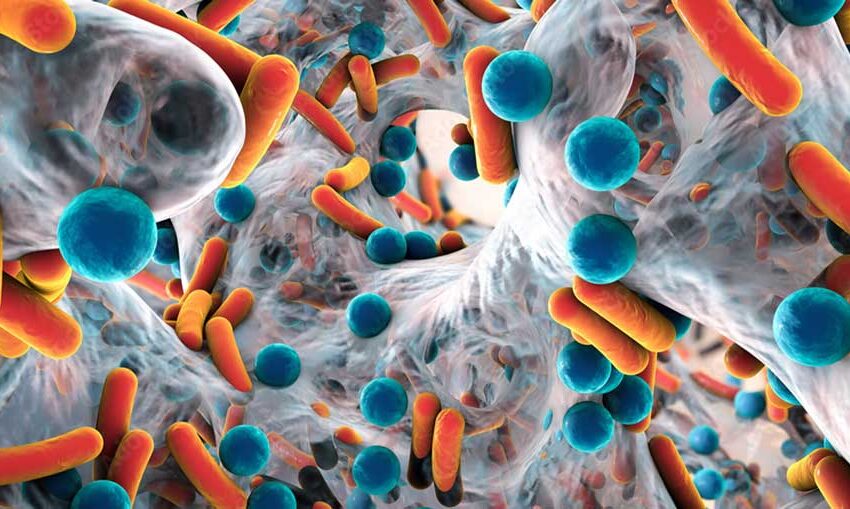
It is easy to picture bacteria as tiny, independent troublemakers floating around, but that’s not quite how they prefer to live. Bacteria often band together, building slick, glue-like communities known as biofilms on surfaces inside the body and out. These microscopic strongholds can form on teeth, the lining of the gut, medical devices, and even your shower drain. The bacteria inside a biofilm protect themselves by creating a slimy shield that keeps antibiotics and the immune system from clearing them out. Over time, these structures can create chronic problems that don’t always show up on a basic test, leading to ongoing inflammation, persistent infections, and even gut issues that just keep coming back, no matter how carefully someone manages their diet or hygiene.
The sticky matrix of a biofilm is made of sugars, proteins, and DNA, working like a fortress to keep the bacteria safe while they multiply quietly. This protective structure can turn minor bacterial annoyances into long-term issues. Imagine a film you can’t scrub off, layered again and again until it becomes too tough to budge. That’s the reality of biofilms and why understanding them is key to understanding certain chronic health concerns that never seem to resolve fully.
Why Biofilms Matter for Your Health
People often find themselves facing persistent gut discomfort, sinus congestion that never clears, or infections that return as soon as treatment ends. In many cases, biofilms are involved, working behind the scenes to protect bacteria from getting wiped out completely. Inside a biofilm, bacteria can share resources, swap genetic material that may include antibiotic resistance, and remain hidden from the body’s usual defense systems. This means that even if a person finishes a round of antibiotics or uses targeted treatments, a portion of bacteria inside the biofilm may survive, ready to flare up again.
Sometimes, the immune system reacts to these protected bacteria, leading to low-level inflammation that lingers and causes fatigue, digestive issues, and a general feeling of unwellness that people struggle to explain. Research shows biofilms may play a role in chronic conditions such as recurrent urinary tract infections, sinusitis, and even in gut issues like irritable bowel syndrome. They can also form on medical devices like catheters and implants, making it harder for healthcare providers to fully clear an infection once it has settled in.
Many people overlook one possible tool that can help break through these barriers when trying to manage these challenges: a biofilm disruptor supplement. This type of targeted supplement can support the body’s ability to dismantle these sticky bacterial layers, allowing the immune system and treatments to reach the bacteria hiding inside. For individuals facing persistent health challenges, using such a supplement under medical guidance may provide a supportive edge in their efforts to feel better.
How Biofilms Form in the Body
Biofilms do not appear overnight. Bacteria first attach loosely to a surface, finding it to be a good spot for colonization, whether on tooth enamel, mucosal linings, or medical tubing. As these bacteria begin to settle in, they start producing a glue-like substance that helps them stick more firmly. From there, they multiply and invite other bacteria to join the party, building a layered community encased in their protective shield.
This structured environment allows bacteria to communicate through chemical signals, coordinate their actions, and exchange resistance traits. It’s a living, breathing city of microbes, protected by its own security system. Within this system, bacteria can enter a dormant state, making them even harder to eliminate since many antibiotics target actively growing bacteria. This means treatment can knock out some of the population, but others remain quietly hidden until the coast is clear.
Biofilms can form in the sinuses, urinary tract, and intestines, often leading to chronic infections that do not resolve with routine treatment. In the mouth, dental plaque is a biofilm that, if left unaddressed, can harden into tartar and contribute to gum disease. Inside the gut, biofilms can shelter harmful bacteria and contribute to ongoing digestive discomfort and inflammation that seem resistant to dietary changes and standard therapies.
Supporting Your Body in Tackling Biofilms
Breaking down biofilms takes a consistent, multi-layered approach that includes lifestyle choices, professional guidance, and sometimes targeted interventions. Gut health, hydration, and diet play important roles, as they can support the immune system and help the body naturally discourage biofilm formation. Managing stress and maintaining consistent sleep patterns help regulate the body’s immune defenses, allowing it to respond appropriately to challenges.
Physical movement also plays an underrated role in supporting the body’s efforts to clear out waste and toxins that can accumulate when biofilms are present. It doesn’t require intense exercise to see benefits. Gentle, regular movement, stretching, and walks can help maintain circulation and lymphatic flow, which are important in supporting sustainable fitness and overall immune health while working to address chronic bacterial issues.
Biofilm-busting efforts often involve guidance from a healthcare provider to ensure safety, especially when working to clear persistent infections or gut imbalances. This approach can support recovery and help individuals move past persistent symptoms that have lingered despite attempts to address them through other methods. The process can take time, as biofilms do not dismantle overnight, but consistent efforts often bring noticeable shifts in how the body feels and functions.
Biofilms and the Bigger Picture of Health
Biofilms represent a fascinating, often hidden layer of complexity in the human body’s interactions with bacteria. While bacteria can be part of a healthy system, biofilms can turn certain bacteria into persistent saboteurs, making recovery harder and inflammation more constant. By understanding how biofilms work and where they can hide, individuals and healthcare providers can address chronic health issues with greater precision.
There is an empowering element in recognizing that what feels like an unsolvable health challenge may have a tangible cause. Addressing biofilms through consistent lifestyle support and targeted interventions when necessary can open pathways to clearer recovery and relief from long-lasting discomfort.
Biofilms might be quiet, but they are far from harmless. Learning how they form and how they can impact the body helps bring clarity to confusing health symptoms and supports a path forward when issues just will not clear on their own.





